Cooper University Health Care Launches a Direct Primary Care Practice in Haddonfield and Welcomes Two Experience Primary Care Providers
Haddonfield, NJ – Cooper University Health Care, the region’s leading academic health system, is proud to partner with experienced family practitioners James J. Runfola, MD, and Leonard V. Ridilla, MD, to announce the launch of a primary care practice that redefines patient-provider relationships. Beginning in April, Cooper will offer Direct Primary Care (DPC), a membership-based model designed to provide unparalleled access and personalized care. Read more.


 Cooper University Health Care’s credit rating for bonds issued by Camden County Improvement Authority was upgraded by S&P Global Ratings (S&P) to an “A“ with a positive outlook. This is the second-straight year S&P has increased Cooper’s credit rating. This follows an A+ credit rating from Fitch Ratings earlier in the month.
Cooper University Health Care’s credit rating for bonds issued by Camden County Improvement Authority was upgraded by S&P Global Ratings (S&P) to an “A“ with a positive outlook. This is the second-straight year S&P has increased Cooper’s credit rating. This follows an A+ credit rating from Fitch Ratings earlier in the month. Ten-year-old Lily Cuticchia of Haddon Township, NJ, is back at it again, opening her heart and hands to help others in need. The fifth-grade student at St. Rose of Lima Catholic School in Haddon Township recently visited Cooper University Hospital to donate more than 600 backpacks filled with blankets and personal care items to help patients at Cooper’s
Ten-year-old Lily Cuticchia of Haddon Township, NJ, is back at it again, opening her heart and hands to help others in need. The fifth-grade student at St. Rose of Lima Catholic School in Haddon Township recently visited Cooper University Hospital to donate more than 600 backpacks filled with blankets and personal care items to help patients at Cooper’s  Cooper University Health Care earned an A+ credit rating from Fitch Ratings (Fitch), an award-winning credit rating agency. This follows two credit upgrades from S&P Global and Moody’s since 2022. This new credit rating represents a double, or two-level, upgrade over Cooper’s 2022 rating.
Cooper University Health Care earned an A+ credit rating from Fitch Ratings (Fitch), an award-winning credit rating agency. This follows two credit upgrades from S&P Global and Moody’s since 2022. This new credit rating represents a double, or two-level, upgrade over Cooper’s 2022 rating.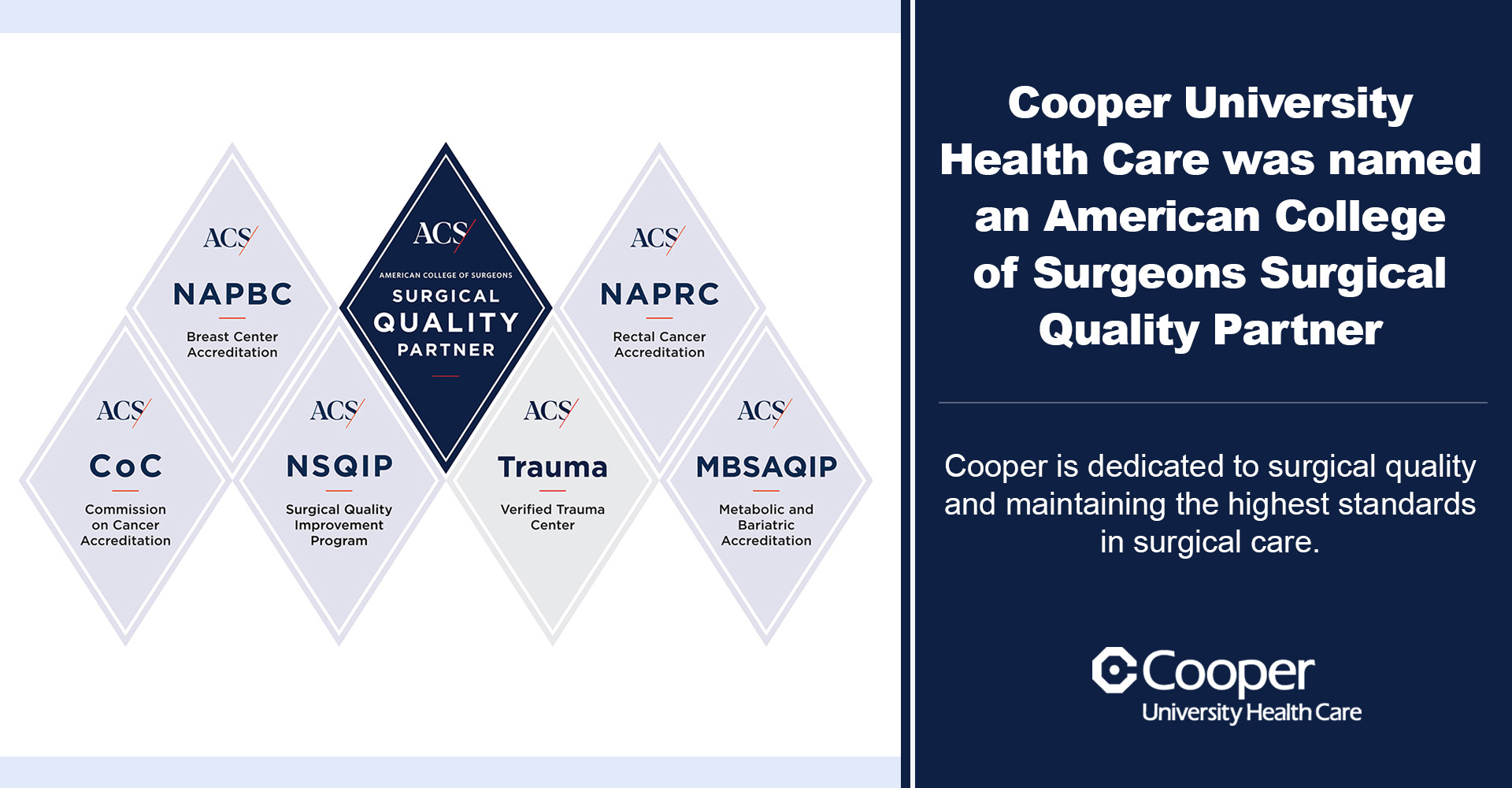 Cooper University Health Care has been recognized as a Surgical Quality Partner by the American College of Surgeons (ACS), highlighting the institution’s unwavering commitment to delivering the highest standards of surgical care.
Cooper University Health Care has been recognized as a Surgical Quality Partner by the American College of Surgeons (ACS), highlighting the institution’s unwavering commitment to delivering the highest standards of surgical care.