Yesterday was the last day of National Drug and Alcohol Facts Week® (NDAFW), an observance that encourages dialogue surrounding substance use and substance use disorder (SUD).
As part of NDAFW, the Cooper University Health Care Center for Healing, a State of New Jersey-designated Medication for Addiction Treatment Center of Excellence (MATCOE), shared content on the Cooper eHealth Blog to educate providers, interdisciplinary care teams, patients, and communities across Cooper, the region, and the state on SUD and available treatments at Cooper:
- How the Cooper Center for Healing Supports Our Patients and Communities
- Medications for Substance Use Disorders, Increasing Access to Treatment, and Decreasing Stigma
- Perinatal Substance Use Care at the Cooper Center for Healing
- Full Coverage Substance Use Disorder and Mental Health Care for Uninsured and Underinsured Patients at the Cooper Center for Healing
Please find additional content on emergency medicine (EM) and hospital-based addiction care services available at Cooper below, and follow MATCOE social media networks on Twitter, LinkedIn, and Instagram for ongoing updates in regard to educational and clinical content and resources available.
Medication for Addiction Treatment Pathways
The Cooper University Health Care Emergency Department Addiction Pathways (CUH EDAP) program, also known as the Cooper ED Bridge program, combines medication for addiction treatment (MAT) by EM physicians and referral to longitudinal care with the goal of facilitating long-term engagement in evidence-based addiction medicine.
In 2016, Cooper’s Division of Addiction Medicine partnered with the ED to train all EM physicians and residents in buprenorphine medication for opioid use disorder (MOUD). The department chair mandated the formerly required “X-waiver” training and certification of all ED medical faculty to promote evidence-based treatment of patients with opioid use disorder (OUD) on the front lines.
In June of 2021, Rachel Haroz, MD, FAACT, Division Head of Addiction Medicine and Toxicology at Cooper and now Medical Director at the Center for Healing, who also serves as Addiction Medicine Medical Director at Salem Medical Center, spearheaded the Salem Medical Center Emergency Department Addiction Pathways (SMC EDAP) program, and in partnership with Patricia Fortunato, Content Manager at the Center for Healing, created a compendium of prescriber education and patient-facing health communication resources, since iterated for the Cooper University Health Care Emergency Department Addiction Pathways (CUH EDAP) program and Southern New Jersey Medication for Addiction Treatment Center of Excellence (MATCOE) networks. Resources are available at snjmatcoe.org.
Under the leadership of Rachel Haroz, MD, FAACT, Division Head of Addiction Medicine and Toxicology and now Medical Director at the Center for Healing, the ED created protocols for assessment of opioid withdrawal, initiation of buprenorphine MOUD, and linkage to maintenance treatment for patients with OUD. Dr. Haroz also initiated universal screening protocols for substance use disorder (SUD) for all pregnant patients in the Cooper ED, and in partnership with what is now the Center for Healing, created a linkage to wrap-around perinatal SUD treatment via the center’s Empowering Mothers to Parent and Overcome with Resilience (EMPOWR) program for pregnant and parenting women struggling with substance use or SUD.
As of 2022, the Cooper ED remains a statewide and national academic and clinical leader in acute access to evidence-based addiction medicine. This acute care innovation has extended to the community with field initiation of buprenorphine post-overdose by Cooper Emergency Medical Services (EMS) paramedics under the leadership of Gerard Carroll, MD, FAAEM, EMT–P, Medical Director of EMS and Division Head of EMS/Disaster Medicine. Individuals who are admitted to the ED for opioid overdose continue to have the ability to be inducted on buprenorphine or methadone with referral for follow-up care at any Center for Healing clinical practice location, CAMcare, or Delaware Valley Medical (Pinnacle Treatment Center). Further the center and EDAP have partnered with Advanced Recovery Systems to build and staff Recovery Village Cherry Hill at Cooper and increase access to inpatient detox and residential services.
Patients who present to the Cooper ED with alcohol use disorder (AUD) are screened, engaged, and are then offered initiation of anti craving medications in the form of oral or depot naltrexone and gabapentin. These patients are linked to the Center for Healing for longitudinal care. The AUD in the ED pathway was implemented in the Cooper ED in the spring of 2021.
The utilization of methadone to treat opioid withdrawal and initiation of treatment for OUD was also standardized in 2021 in the Cooper ED and by the inpatient consult team. Further, across 2022, the team completed a retrospective evaluation of methadone initiation in the ED with linkage to treatment at Pinnacle Treatment Center, collecting visit attendance data post-hospital discharge. In this study, the team—led by Samantha Huo, MD, recent Cooper Addiction Medicine Fellowship graduate, and overseen by Dr. Haroz—describes the utilization of the Code of Federal Regulations (CFR) Title 21 1306.07 (b), also known as the “72-hour rule,” to initiate methadone for OUD in the Cooper ED. The manuscript and accompanying algorithm was accepted for publication and is in press with the Journal of Emergency Medicine as of January of 2023.
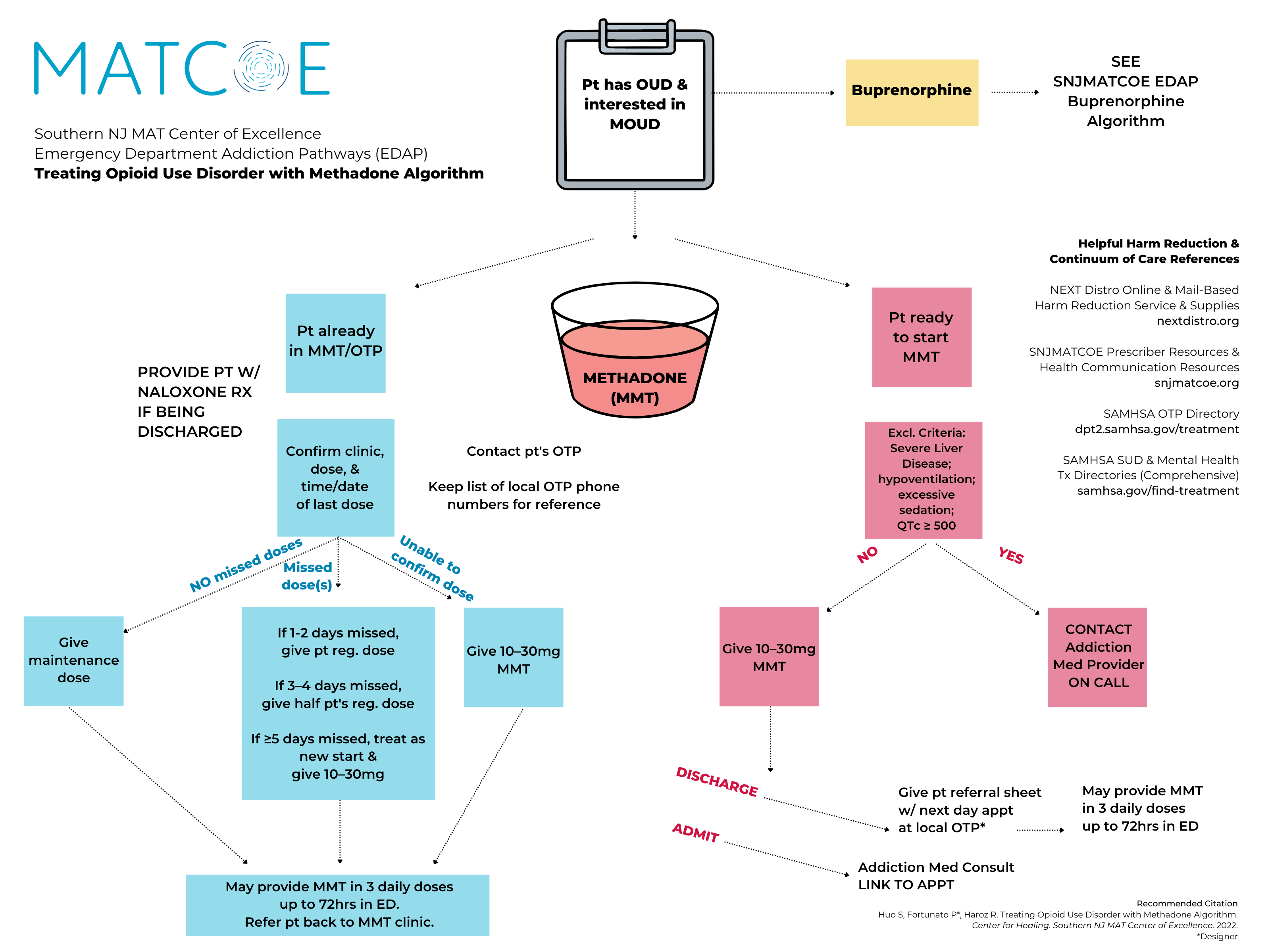
View the algorithm at cooperhealth.edu/fellowships/addiction-medicine/quality.
Emergency Medical Services Treatment Pathways
Since 2019, Cooper’s Buprenorphine Field Initiation of ReScue Treatment (Bupe FIRST EMS), as the program is now known, was the first program nationally, and remains the only EMS agency in the state, to provide buprenorphine MOUD in the field. Cooper EMS, Addiction Medicine, and Toxicology Divisions collaborated to write a protocol for buprenorphine administration in the field, well-received and proliferated across the nation. Investigators, led by Dr. Carroll and overseen by Dr. Haroz, published a case series to describe the intervention and most recently, in September of 2022, published a retrospective cohort study in Annals of Emergency Medicine to determine the impact of this program on subsequent overdose and treatment retention, in collaboration with researchers from the Johns Hopkins Bloomberg School of Public Health. Additionally, investigators have presented the protocol at regional and national conferences, and the protocol has since been adapted by EMS across the nation and gained recognition in various press.
Addiction Consultation Services Team
Since its inception, the Cooper Addiction Medicine team, now known as the Center for Healing team, has offered expert-level addiction care for patients with complex medical needs who are hospitalized at Cooper. Over time, the need and request for hospital consults grew, and in 2017, the Division of Addiction Medicine piloted a full-time consult service, now known as the CUH ACT (Cooper University Health Care Addiction Consultation Services Team). The ACT is now fully staffed with addiction medicine board-certified physicians, addiction medicine fellows, advanced practice providers, a clinical alcohol and drug counselor who also serves as inpatient care coordination supervisor, and behavioral medicine psychologists. The ACT is a teaching service run by Matthew Salzman, MD, Medical Director of Inpatient Consult Services for Addiction Medicine and Medical Director of Research at the Center for Healing.
The center’s physicians are also working with other hospital divisions on quality improvement (QI) projects and protocols for treating common illnesses. The center is training more hospitalist providers in basic addiction medicine care, and as an organization, the team is working to ensure that all hospital medicine providers offer MOUD to OUD patients. As this training has increased, the number of buprenorphine prescriptions written by non-addiction medicine providers have also increased, enabling MOUD as part of routine care.
Most recently, in January of 2023, as part of a content and clinical collaboration and overseen by Dr. Salzman, the center produced a new inpatient clinician education tool for inpatient nurses—a screening, brief intervention, and referral to treatment (SBIRT) algorithm for inpatient settings, since iterated for the team’s Southern New Jersey MATCOE networks.

Prescriber and clinician education and health communication resources are available at snjmatcoe.org.
