September is Sepsis Awareness Month. In the 20 seconds it takes you to read this, another person in the U.S. will be diagnosed with sepsis. For the 1.7 million people diagnosed with sepsis each year, rapid recognition and treatment are crucial to their survival. Similar to strokes and heart attacks, sepsis is a medical emergency that requires rapid diagnosis and treatment.
Every year, an estimated 49 million people worldwide are affected by sepsis. In the U.S., 350,000 adults die from sepsis each year. More people die from sepsis than from opioid overdoses, breast cancer, and prostate cancer combined. It is the leading cause of death in U.S. hospitals.
Sepsis is the body’s overwhelming and life-threatening response to infection that can lead to tissue damage, organ failure, and death. In other words, it’s your body’s overactive and toxic response to an infection. Sepsis can lead to severe sepsis and septic shock.
Your immune system usually works to fight germs (bacteria, viruses, fungi, or parasites) to prevent infection. If an infection does occur, your immune system will try to fight it, although you may need help from medications such as antibiotics, antivirals, antifungals, and antiparasitics. However, for reasons researchers don’t understand, sometimes the immune system stops fighting the “invaders,” and begins to turn on itself. This is the start of sepsis.
Some people are at higher risk of developing sepsis because they are at higher risk of contracting an infection. This includes people who are very young (infants) or very old, those with chronic illnesses, and those with a weakened or impaired immune system. People who are malnourished can also contract infections more easily.
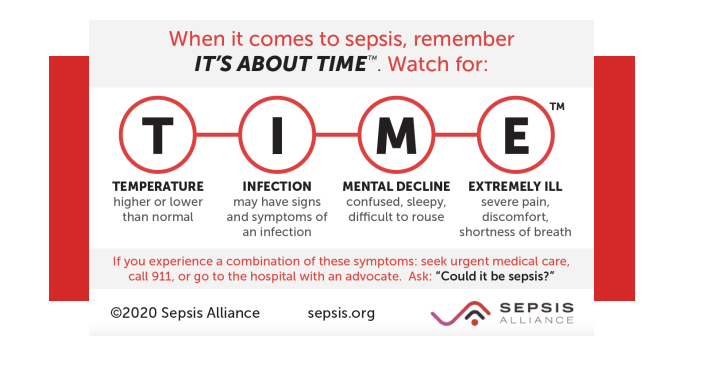
Patients are diagnosed with sepsis when they develop a set of signs and symptoms related to sepsis. Sepsis is not diagnosed based on an infection itself. If you have more than one of the symptoms of sepsis, especially if there are signs of an infection or you fall into one of the higher risk groups, your doctor will likely suspect sepsis.
Sepsis progresses to severe sepsis when, in addition to signs of sepsis, there are signs of organ dysfunction, such as difficulty breathing, low or no urine output, abnormal liver tests, and changes in mental status. Nearly all patients with severe sepsis require treatment in an intensive care unit.
Septic shock is the most severe level of sepsis and is diagnosed when your blood pressure drops to dangerous levels.
Sepsis is the number one cost of hospitalization in the U.S. Costs for acute sepsis hospitalization and skilled nursing are estimated to be $62 billion annually. This is only a portion of all sepsis-related costs – for many people, there are substantial additional costs after they are discharged from the hospital.
The average cost per hospital stay for sepsis is double the average cost per stay across all other conditions. Sepsis is the primary cause of readmission to the hospital, costing more than $3.5 billion each year.
Studies investigating survival and sepsis deaths have reported slightly different numbers, but it appears that on average, approximately 30% of patients diagnosed with severe sepsis do not survive. Up to 50% of survivors suffer from post-sepsis syndrome, a condition that includes physical and/or psychological long-term effects.
Early detection and treatment are essential for surviving sepsis and limiting disability for survivors.
